Understanding Knee Arthritis
Knee arthritis is a common and progressive joint condition that affects millions of people worldwide, particularly those above the age of 50. It occurs when the protective cartilage that cushions the knee joint gradually wears away, leading to pain, swelling, stiffness, and reduced mobility.
The knee is one of the largest and most complex joints in the human body. It bears most of our body weight during activities such as walking, running, and climbing stairs. Over time, or due to injury and other factors, the smooth cartilage that allows the knee bones to glide easily can deteriorate. As this protective layer wears out, the bones begin to rub against each other, causing inflammation, discomfort, and loss of movement.
Knee arthritis can develop slowly over several years, and early diagnosis is the key to slowing its progression and preserving joint health.
Types of Knee Arthritis
There are several forms of arthritis that can affect the knee joint, including:
-
Osteoarthritis (OA):
The most common type, often referred to as “wear-and-tear” arthritis. It develops gradually with age or due to overuse, leading to cartilage breakdown and joint degeneration. -
Rheumatoid Arthritis (RA):
An autoimmune disease where the immune system mistakenly attacks the joint lining, causing chronic inflammation and eventual cartilage and bone damage. -
Post-Traumatic Arthritis:
This occurs after a knee injury such as a fracture, ligament tear, or meniscus damage. Even when the injury heals, the joint may develop arthritis years later due to abnormal stress distribution.
Understanding the type of arthritis helps your doctor tailor a treatment plan that best fits your condition.
Common Causes of Knee Arthritis
Several factors contribute to the development of knee arthritis, and often a combination of these leads to its onset:
-
Aging: Natural wear and tear of cartilage with age is the most common cause.
-
Obesity: Excess body weight increases stress on the knee joints, accelerating cartilage breakdown.
-
Previous Knee Injuries: Fractures, ligament tears, or meniscus injuries can lead to premature arthritis.
-
Genetic Predisposition: Family history can increase the likelihood of developing arthritis.
-
Occupational or Lifestyle Stress: Jobs or activities involving repetitive squatting, kneeling, or heavy lifting put extra pressure on the knees.
-
Poor Posture or Joint Alignment: Misalignment of the legs (bowlegs or knock-knees) can cause uneven joint wear.
While some causes, such as genetics and aging, cannot be changed, lifestyle modifications can significantly reduce risk and slow progression.
Recognizing the Symptoms
Knee arthritis typically develops gradually, and symptoms may initially appear mild before becoming more severe over time. Common signs include:
-
Pain: A dull, aching pain in or around the knee, often worse after activity.
-
Stiffness: Especially noticeable in the morning or after sitting for long periods.
-
Swelling: Caused by inflammation or excess joint fluid.
-
Reduced Range of Motion: Difficulty bending or straightening the knee fully.
-
Grinding or Clicking Sound (Crepitus): Due to rough joint surfaces rubbing together.
-
Difficulty with Daily Activities: Pain while climbing stairs, standing from the floor, or walking long distances.
If these symptoms persist, it’s important to consult an orthopedic specialist for an accurate diagnosis and early management.
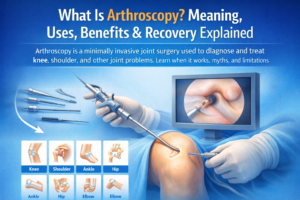
How Knee Arthritis Is Diagnosed
Diagnosis involves a thorough clinical evaluation that includes:
-
Medical History: To understand the pattern of pain, stiffness, and physical limitations.
-
Physical Examination: Assessing swelling, tenderness, and range of motion.
-
Imaging Tests: X-rays can reveal joint space narrowing and bone changes, while MRI scans provide detailed views of cartilage, ligaments, and soft tissues.
Early diagnosis is crucial because intervention at the initial stages can prevent further joint damage and reduce the need for surgery later.
Non-Surgical Treatment Options
In the early and moderate stages of knee arthritis, most patients can manage symptoms effectively without surgery. Treatment focuses on relieving pain, improving mobility, and slowing cartilage wear.
1. Lifestyle Modifications
-
Maintain a healthy weight to reduce pressure on the knees.
-
Avoid high-impact activities like running or jumping; opt for low-impact exercises.
2. Physiotherapy and Exercise
-
Strengthening the thigh (quadriceps) and hip muscles provides better support to the knee.
-
Flexibility and balance exercises improve stability and reduce stiffness.
3. Medications
-
Over-the-counter pain relievers or anti-inflammatory drugs may help reduce pain and swelling.
-
Supplements such as glucosamine and chondroitin are sometimes used to support cartilage health.
4. Injections
-
Corticosteroid or hyaluronic acid injections may provide temporary pain relief and improve joint function.
5. Assistive Devices
-
Knee braces, walking sticks, or orthotic shoe inserts can reduce strain and improve alignment.
These conservative measures are most effective when started early and maintained consistently under professional supervision.
Prevention: Protecting Your Knees for the Long Term
While aging is inevitable, there are several proactive steps you can take to prevent or delay knee arthritis:
-
Maintain a Healthy Weight: Even a small reduction in body weight can significantly reduce stress on the knees.
-
Engage in Regular Exercise: Activities like swimming, cycling, and walking help strengthen muscles without overloading the joints.
-
Practice Good Posture: Proper alignment during sitting, standing, and walking minimizes undue pressure.
-
Avoid Overuse: Alternate between sitting and standing, and avoid repetitive strain from squatting or lifting.
-
Wear Proper Footwear: Supportive shoes help maintain correct leg alignment.
-
Protect Against Injuries: Warm-up before exercise and use knee guards if necessary during sports or heavy physical activity.
Early preventive measures can delay or even avoid the need for surgical intervention later in life.
When to Consider Surgery
If pain persists despite comprehensive non-surgical management, surgical options such as Total Knee Replacement (TKR) or Partial Knee Replacement (PKR) may be considered. These procedures replace the damaged cartilage and bone surfaces with artificial implants, restoring movement and relieving pain.
Your orthopedic surgeon will assess factors like joint damage, lifestyle, and overall health to recommend the most suitable treatment approach.
Frequently Asked Questions (FAQs)
Q1. Can knee arthritis be cured without surgery?
A: In early stages, knee arthritis can often be managed effectively without surgery through weight control, physiotherapy, medications, and lifestyle modifications. Surgery is only required in advanced cases.
Q2. Does walking worsen arthritis?
A: No. In fact, moderate walking helps maintain joint mobility and strengthens muscles. Avoiding all activity can make stiffness and pain worse.
Q3. Is arthritis hereditary?
A: Yes, genetics can increase your risk. If arthritis runs in your family, maintaining a healthy lifestyle and regular exercise can help delay its onset.
Q4. What foods help with arthritis?
A: A balanced diet rich in omega-3 fatty acids, fruits, vegetables, and whole grains helps reduce inflammation and supports joint health.
Q5. When should I see a doctor for knee pain?
A: Persistent pain, stiffness, swelling, or difficulty with daily tasks lasting more than a few weeks should prompt a consultation with an orthopedic specialist.
Conclusion
Knee arthritis is a progressive yet manageable condition. Understanding its causes, recognizing early symptoms, and adopting preventive measures can make a significant difference in maintaining long-term joint health.
By staying active, maintaining a healthy weight, and seeking timely medical advice, patients can delay the progression of arthritis, minimize discomfort, and maintain an active lifestyle well into later years.
If you are experiencing persistent knee pain or stiffness, consult an experienced orthopedic surgeon for a comprehensive evaluation and personalized treatment plan. Early intervention is the key to preserving mobility and preventing future complications.